The Main Cause of Nail Fungus
(Onychomycosis)
Onychomycosis, or nail fungus, is a common fungal infection that anyone can get. However, some people have a higher risk of contracting this pesky fungus than others. Understanding lifestyle risks that can put you at a higher risk of getting nail fungus can help you avoid contracting it and prompt you to get seek medical attention when you note symptoms.
Nail fungus is caused by microscopic organisms, fungi that, when they multiply under your finger or toenails, cause a nail infection. It is commonly caused by:
- Frequently wearing sweaty or moist socks
- Walking barefoot in shared warm, moist areas like a locker room, pool deck, or shower
- Sharing towels or unsanitized nail clippers
- Skin-to-skin contact with someone who has Onychomycosis, athlete's foot, or ringworm
Your age, lifestyle, and overall health all play a role in whether or not you'll get a fungal infection under your nails. Onychomycosis is easily treatable when caught early and diagnosed by a reliable diagnostic lab like Meridian Diagnostic Lab

Understanding Onychomycosis
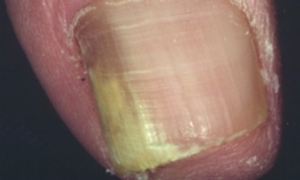
 The most obvious symptom of nail fungus is a thickened, yellow toe or fingernail. The nail may also have white spots or streaks and separate from the nail bed. A contagious mold called dermatophyte causes the most common type of nail fungus, tinea unguium, also called Onychomycosis.
The most obvious symptom of nail fungus is a thickened, yellow toe or fingernail. The nail may also have white spots or streaks and separate from the nail bed. A contagious mold called dermatophyte causes the most common type of nail fungus, tinea unguium, also called Onychomycosis.
While it's most common in the toes, it can also affect the fingers. It's extremely contagious, so an outbreak in a shared community, like an athletic club or nursing home, may mean everyone who lives there or uses the facility will pick up the fungus.
Early treatment for Onychomycosis is essential, especially for people who are elderly or in poor overall health. While it's not usually painful, unless the nail separates from the bed, it is unsightly and will continue to spread if not eliminated. Spreading nail fungus could cause someone to lose their nail, which can be dangerous.
Common Causes of Onychomycosis
 Skin-to-skin contact with someone with an Onychomycosis infection is the most common transmission method. Another common way to pick up an Onychomycosis infection is by walking barefoot in warm and moist areas, like a sauna, pool deck, public shower, or locker room. These conditions cause fundi to thrive. Sharing nail clippers without properly sanitizing them or sharing towels can also transmit the fungus from one person to another.
Skin-to-skin contact with someone with an Onychomycosis infection is the most common transmission method. Another common way to pick up an Onychomycosis infection is by walking barefoot in warm and moist areas, like a sauna, pool deck, public shower, or locker room. These conditions cause fundi to thrive. Sharing nail clippers without properly sanitizing them or sharing towels can also transmit the fungus from one person to another.
You don't have to interact with another person to contract Onychomycosis, though. If your socks and shoes get sweaty and you don't keep your socks clean and dry, or if your hands are frequently wet or moist, fungi can develop independently.
Poor hygiene, like not scrubbing underneath the nails regularly, or damage and trauma to the nails, like wearing tight shoes or keeping sweaty socks on the feet and not changing them, can also cause you to develop nail fungus.
Risk Factors for Onychomycosis
Although anyone can contract nail fungus, some people are likelier to have it than others. If you are;
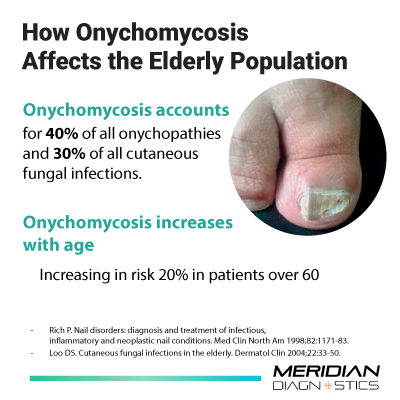
- Elderly
- In poor health or immunocompromised
- Live in a shared space with shared bathroom, shower, or pool facilities
then you stand a much higher chance of contracting Onychomycosis than other people
Prevention and Treatment of Onychomycosis
 Diagnosis of Onychomycosis starts with a visual exam by a healthcare provider, who looks at the affected nails and considers your symptoms. Often, they will scrape a small sample of the fungus from beneath your nail, sending it to a diagnostic lab to determine the strain of fungus. Your doctor may also test for infection.
Diagnosis of Onychomycosis starts with a visual exam by a healthcare provider, who looks at the affected nails and considers your symptoms. Often, they will scrape a small sample of the fungus from beneath your nail, sending it to a diagnostic lab to determine the strain of fungus. Your doctor may also test for infection.
Toenail fungus may not cause infection on its own, but the damage that it does to the nail beds can leave them vulnerable to infection from other sources.
Viewing the fungi cells under a microscope confirms the toenail fungus diagnosis. Once the diagnosis is confirmed, the lab may look for the presence of other types of infections that the person may have picked up due to the deterioration of the nail bed caused by the fungus.
Toenail fungus is stubborn and resistant to treatment, which means that many people may need months of consistent treatment to eliminate the treat tinea and prevent it from recurring. Some of the most common options are:
- Taking a daily oral antifungal medication, like Lamisil®, Diflucan®, or Sporanox®. However, these may interfere with other medications and can affect the liver
- Application of topical antifungal medication, most effective when paired with oral medication
- Laser treatment for the most stubborn fungal infections
Once the fungus is gone, cleanliness and keeping the hands and feet dry are the best ways to prevent it from returning. Maintaining clean, dry, and sanitized shared spaces, like pools and locker rooms, is critical to reducing the presence of the mold that causes Onychomycosis. Not sharing towels or nail clippers or sanitizing clippers between users also prevents the spread of the fungus.
Don't Delay Diagnosis and Treatment If You Suspect Nail Fungus
Nail fungus is a very contagious form of fungal infection that can deteriorate the nail beds. It's more common in ties than fingers but left unchecked, it can cause serious or permanent damage to the affected nail and nail bed.
Early diagnosis is important for proper treatment. The earlier you catch stubborn nail fungus, the less time you may need to take oral medications or apply topical creams. If you suspect that you or people under your care have toenail fungus, marked by yellow, thick toenails, and separation from the nail bed, you may need to have samples tested to confirm the visual diagnosis.
Seek professional medical attention for toenail fungus, including diagnostic testing from a medical lab you trust – Meridian Diagnostics.


