Medicaid Changes: Challenges Amidst Post-COVID

The conclusion of the COVID-19 pandemic has triggered a wave of reconsiderations for Medicaid enrollees across the United States. As eligibility reviews resume, some states have swiftly halted health care coverage, leading to the drop of over a million people from the program. While the process is mandated by the federal government, concerns have arisen about its efficiency and impact on eligible individuals, especially those with medically complex conditions. In this article, we explore the complexities and challenges faced by states and Medicaid enrollees in the aftermath of the pandemic.
Post-Pandemic Medicaid Reconsideration
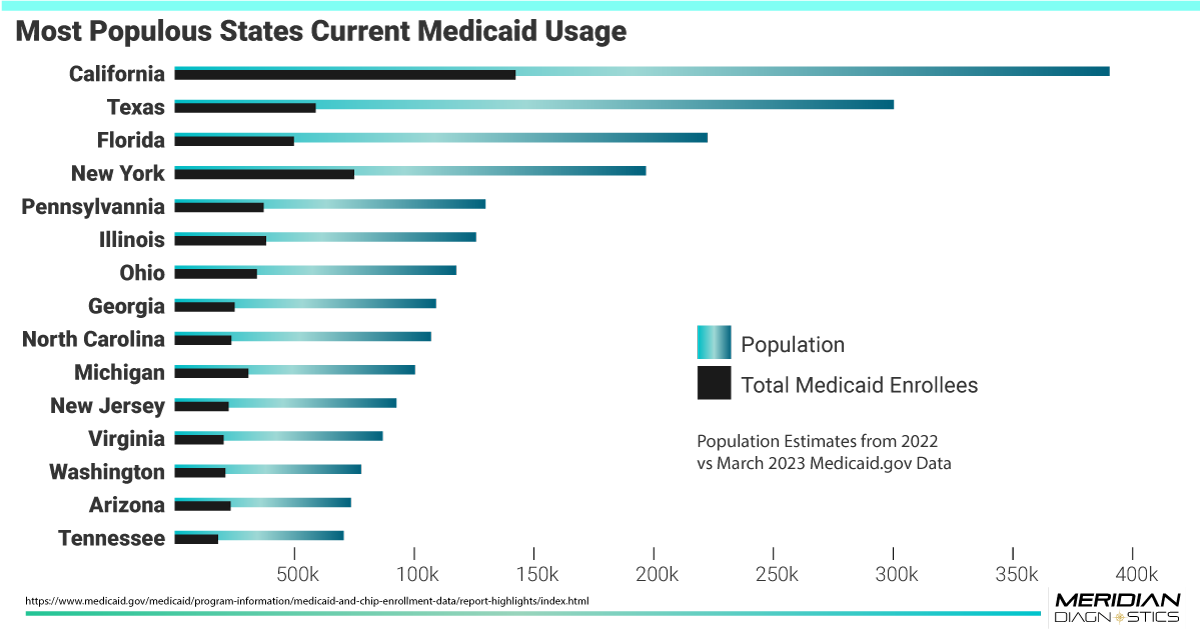
 The end of the pandemic has ushered in a critical phase for Medicaid, as states are required to conduct eligibility reviews for all enrollees. Despite being a necessary step, the implementation of this process has been met with varied efficiency across different states. Reports indicate that over 1.5 million people have been removed from Medicaid rolls in more than two dozen states that started the review process in April or May. Florida, leading the numbers with several hundred thousand people dropped, highlights the magnitude of the issue.
The end of the pandemic has ushered in a critical phase for Medicaid, as states are required to conduct eligibility reviews for all enrollees. Despite being a necessary step, the implementation of this process has been met with varied efficiency across different states. Reports indicate that over 1.5 million people have been removed from Medicaid rolls in more than two dozen states that started the review process in April or May. Florida, leading the numbers with several hundred thousand people dropped, highlights the magnitude of the issue.
Challenges Faced by Medicaid Enrollees
For many Medicaid enrollees, the eligibility redetermination process has proven to be a complex and frustrating journey. Amidst the resumption of eligibility reviews, individuals have faced difficulties in providing necessary paperwork, resulting in coverage terminations. Despite receiving multiple contact attempts from state agencies through texts, emails, and phone calls, a significant number of enrollees have been non-responsive to the renewal process, inadvertently losing their coverage.
Amidst the implementation of Medicaid reconsideration across various states, personal stories of individuals grappling with the consequences of coverage loss shed light on the human impact of these changes. These heart-wrenching experiences highlight the challenges faced by vulnerable populations and underscore the need for a balanced approach in the eligibility review process.
- Charlotte Douberley, a 2-year-old with cystic fibrosis, found herself at risk of losing Medicaid coverage, contrary to expectations. Her mother, Chianne Douberley, was shocked to discover that Charlotte's coverage was set to be terminated, leaving her without health insurance since May 31. The situation compounded when Charlotte's vital medication, costing $26,000 a month, was set to run out before her new coverage could begin. Chianne Douberley tirelessly sought solutions, facing emotional and financial strain in her pursuit of support for her daughter's healthcare needs.
- For Jennifer Mojica, Medicaid redeterminations brought unforeseen challenges. Initially told that she no longer qualified due to a miscalculated income, she eventually resolved the issue. However, new hurdles emerged when her son's coverage was unexpectedly dropped. Despite efforts to rectify the situation, Ms. Mojica encountered a series of administrative obstacles, leading to frustration and uncertainty about her family's healthcare coverage.
- Gary Rush, a resident of Pittsburgh, faced the unsettling prospect of losing Medicaid coverage due to perceived ineligibility based on retirement accounts. Despite not drawing from these accounts, he was notified of coverage termination. Rush sought an appeal with the assistance of an advocacy group, but the uncertainty remained. The looming deadline to reduce savings placed immense pressure on him, especially given the significant cost of his essential medication, which amounted to about $700 a month. For individuals like Mr. Rush, the threat of losing critical healthcare coverage adds stress and concern to their daily lives.
Responding to criticism, Arkansas Governor, Sarah Huckabee Sanders, defended the state's Medicaid process, countering the criticism by stating, "Those who do not qualify for Medicaid are taking resources from those who need them[...] But the pandemic is over – and we are leading the way back to normalcy."
As states proceed with eligibility reviews, it is essential to recognize the human toll of these changes and ensure that measures are in place to protect vulnerable populations. A compassionate and empathetic approach to the eligibility review process is necessary to safeguard access to vital healthcare services for those who rely on Medicaid as a lifeline during times of need.
Impact on Medically Complex Individuals
The implications of Medicaid reconsideration are particularly severe for medically complex individuals, including children with chronic illnesses. Previously, the federal government's prohibition on removing people from Medicaid during the pandemic provided a safety net for vulnerable populations. However, with the review process in full swing, there are concerns about eligible individuals losing their coverage temporarily, potentially leading to adverse health outcomes.
Striving for a Balanced Approach
While eligibility reviews are essential for the effective management of Medicaid programs, there is a need for a balanced approach that considers the challenges faced by enrollees. The rush to complete the review process has raised concerns about eligible individuals inadvertently losing their coverage due to procedural reasons, such as failure to respond or provide required documents.
Conclusion
The post-COVID era has brought significant changes to Medicaid programs across the nation. With eligibility reviews underway, states face the challenge of efficiently navigating a backlog of cases, while Medicaid enrollees navigate the complexities of providing required paperwork amidst life changes. Striking a balance between conducting necessary reviews and ensuring that eligible individuals retain access to vital healthcare coverage remains crucial. As the process continues, stakeholders must collaborate to mitigate challenges and protect vulnerable populations, including medically complex individuals, from disruptions in their healthcare coverage.

