Dermatophytes, Yeasts, and Molds: How Do We Treat Them?
Fungal infections of the skin and nails are common medical conditions that can be caused by various fungi, including dermatophytes, yeasts, and molds. Rapid and accurate diagnosis of these infections is essential for effective treatment. Polymerase Chain Reaction (PCR) molecular testing has emerged as a powerful tool in clinical laboratories for the detection of these fungal pathogens. In this blog post, we will explore the similarities and differences between dermatophytes, yeasts, and molds when detected through PCR molecular testing. Additionally, we will discuss treatment recommendations for each of these fungal infections.
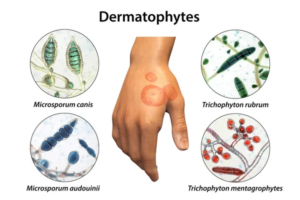
I. Dermatophytes
Dermatophytes are a group of pathogenic fungi that infect the skin, hair, and nails. The most common genera include Trichophyton, Microsporum, and Epidermophyton. Dermatophyte infections are known as dermatophytosis or tinea infections, and they are responsible for conditions like athlete's foot, jock itch, and ringworm.
Detection via PCR Molecular Testing:
PCR molecular testing for dermatophytes typically involves the amplification of specific fungal DNA fragments from clinical samples, such as skin scrapings or nail clippings. This method allows for highly sensitive and specific detection of dermatophytes, even in cases where conventional culture methods may fail.
Treatment Recommendations:
- Topical Antifungal Agents: For mild to moderate dermatophyte infections, topical antifungal creams, lotions, or powders are often effective. Commonly used agents include terbinafine, clotrimazole, and miconazole. These should be applied daily until the infection resolves, which may take several weeks.
- Oral Antifungal Medications: In cases of severe or recalcitrant dermatophyte infections, oral antifungal drugs like terbinafine and itraconazole may be prescribed. These are typically taken for a few weeks to a few months, depending on the extent and severity of the infection.
- Preventative Measures: It's important to educate patients on proper hygiene, as well as the importance of keeping the affected area dry and clean. Patients should also be advised to avoid sharing personal items, such as towels, to prevent the spread of infection.
II. Yeasts
Yeasts are unicellular fungi that are commonly found on the skin, mucous membranes, and in various environmental sources. While many yeasts are harmless, some species can cause opportunistic infections, particularly in individuals with compromised immune systems. Candida species are the most common pathogens responsible for yeast infections in clinical settings.
Detection via PCR Molecular Testing:
PCR molecular testing for yeasts involves the detection of specific genetic sequences unique to the yeast species in question. This method is highly sensitive and can accurately identify the causative yeast in clinical samples, such as swabs or biopsies.
Treatment Recommendations:
- Topical Antifungal Agents: For localized yeast infections, topical antifungal creams, ointments, or suppositories are usually sufficient. Clotrimazole, miconazole, and nystatin are commonly prescribed for these purposes. Treatment duration may vary but typically lasts for a week or more.
- Oral Antifungal Medications: In cases of recurrent or systemic yeast infections, oral antifungal medications like fluconazole, itraconazole, or ketoconazole may be recommended. The duration of treatment is typically longer, lasting from several days to weeks.
- Management of Underlying Conditions: For patients with recurring yeast infections, it's essential to address any underlying medical conditions that may be contributing to susceptibility, such as diabetes or immunosuppression.
- Lifestyle Modifications: Patients should be advised to maintain proper hygiene, avoid tight-fitting clothing, and make dietary adjustments (if appropriate) to reduce sugar intake, as high sugar levels can promote yeast overgrowth.
III. Molds
Molds are multicellular fungi that are typically found in the environment, and they are not common causes of clinical skin infections. However, certain molds can occasionally infect the skin, particularly in individuals with compromised immunity or traumatic skin injuries. One example is the fungus Aspergillus.
Detection via PCR Molecular Testing:
PCR molecular testing for molds is similar to that for dermatophytes and yeasts. It involves the amplification of specific DNA sequences unique to the mold species. This method provides a highly sensitive and specific means of detecting mold pathogens.

Treatment Recommendations:
- Antifungal Medications: The treatment of mold infections is more challenging than that of dermatophytes and yeasts. Antifungal drugs such as itraconazole, voriconazole, or posaconazole are typically used. The choice of medication depends on the specific mold species and the patient's clinical condition.
- Surgical Intervention: In some cases, surgical debridement or removal of infected tissue may be necessary, especially if the mold infection has caused extensive tissue damage.
- Management of Underlying Conditions: Treating the underlying condition that makes the patient susceptible to mold infections, such as immunosuppression, is crucial.
- Environmental Measures: Reducing the patient's exposure to environmental sources of molds is essential to prevent recurrent infections. This may involve addressing water damage in the home or workplace and using appropriate protective measures.
Meridian Diagnostics Is Here to Help!
PCR molecular testing has revolutionized the diagnosis of fungal infections in clinical laboratories. Meridian Diagnostics' lab-developed-test (LDT) utilizes the PCR method for molecular testing of onychomycosis (nail fungus) which allows for rapid and accurate identification of dermatophytes, yeasts, and molds. The Colorado based laboratory is capable of resulting these fungal specimens on average of 36 hours once the specimens are delivered to the lab in Colorado Springs. Each group of fungi presents unique challenges and considerations for treatment are included in the "Anti-fungal Treatment Recommendations" section of every fungal report, a feature many clients have shown much appreciation for.
Dermatophytes are common causes of skin and nail infections and can be effectively treated with topical or oral antifungal agents. Yeasts, such as Candida species, can cause localized or systemic infections and are managed with antifungal medications. Molds are less common pathogens, but when they do infect the skin, treatment can be more challenging, often requiring antifungal drugs and sometimes surgical intervention.
In all cases, it's essential to tailor the treatment to the specific fungal pathogen, the severity of the infection, and the patient's clinical condition. Additionally, addressing underlying medical conditions and promoting good hygiene practices are essential components of a successful treatment plan. Patients should be educated about the importance of adherence to treatment and preventative measures to reduce the risk of recurrent infections. Contact us today to learn how Meridian Diagnostics can help you treat cases of nail fungus effectively.

